Clinical Conditions
Dilated Cardiomyopathy in Dobermans - CALL TO ALL DOBERMANS
 Dilated Cardiomyopathy
Dilated Cardiomyopathy
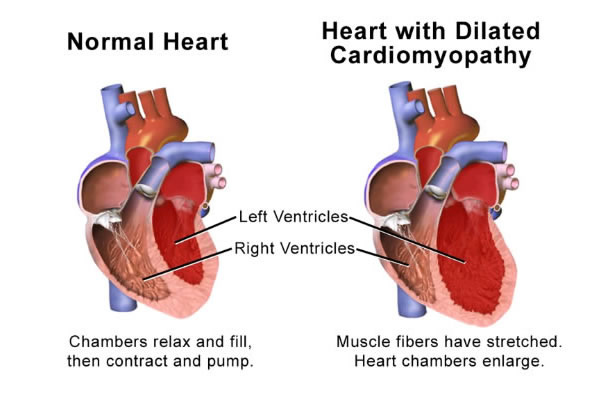
Dilated cardiomyopathy leading to heart failure is a devastating disease. The heart muscle becomes diseased, the muscle fibres die and the heart loses its ability to beat properly.
All large dog breeds are susceptible. The disease’s severity varies with the breed and unfortunately in Dobermans, the disease progresses quickly once symptoms develop and many will only live a few months after diagnosis even on treatment.
Recent work by an international group of top veterinary cardiologists has shown that treatment of Dobermans with pimobendan when they have measurable changes on their echocardiography examination (heart scan), but prior to developing visible symptoms of heart failure (symptoms include breathlessness coughing collapse) significantly prolongs life and quality if life by delaying the onset of heart failure.
We recommend regular echocardiography examinations (heart scans) in Dobermans from 4 years old to determine whether treatment would be beneficial or not.
Please contact the practice on 01492 531448 if you are interested in an examination.
Hyperthyroidism in the Cat
Please download the latest information about this condition here
Osteoarthritis Management
Osteoarthritis is a degenerative disease of joints most commonly seen in older large breed dogs or following joint injury or disease. Any joint can be affected but arthritis most frequently involves the hips, stifles and elbows.
Clinical signs can vary widely from a mild stiffness to severe lameness. Owners may also notice reduced muscle over the affected area. As a disease of older dogs the signs can often be mistaken simply for slowing down with age. In these patients a real improvement can sometimes be seen once treatment has started.
Treatment Options
Each patient must be treated as an individual when managing arthritis as there are many issues to consider. These include severity of signs, bodyweight, number/ type of joints affected, age, activity levels and other concurrent illnesses.
For example a younger active Labrador with hip arthritis would be managed differently from an older dog with arthritis in all four limbs. In most cases a combination of treatments are used.
- Weight control – excess bodyweight can put extra strain on joints and so weight loss can make a major difference to mobility in arthritic animals. Recent studies have also shown links between excess fatty tissue and increased inflammation in joints.
- Controlled Exercise – Exercise is important to maintain muscle support for joints but should not be excessive. The amount of exercise each day should be fairly consistent and not cause excessive stiffness the following day. Activities like swimming can provide low impact exercise and some clients can be referred for hydrotherapy. Fast running and chasing toys can put extra strain on joints and should generally be avoided.
- Joint Supplements (glucosamine, chondroitin, essential fatty acids) – Glucosamine and chondroitin are natural building blocks of healthy cartilage and are needed for repair in arthritic joints. Essential fatty acids have been found to be most the useful, of this group of products, in helping to reduce joint inflammation. In some patients these can make a significant difference to clinical signs without the risk of major side effects. Although they are available for humans these preparations are not always suitable for or effective in animals. We would recommend animal licensed products only
- Anti-inflammatory Painkillers – The most commonly used type of painkillers for arthritis are Non Steroidal Anti-Inflammatory Drugs (NSAIDs). They block part of the inflammatory pathway involved in joint pain. In cases with moderate to severe lameness they can be a very important part of arthritis management. Within the broad category of NSAIDs there are several different drugs. The choice of which to use depends on the individual as some will respond better to one than another. Similarly some animals will develop side effects on one drug but will tolerate another well. Side effects are usually mild, including vomiting or diarrhoea, but in a small minority of cases the drugs can affect liver and kidney function. For this reason we usually recommend a screening blood test prior to use of long term anti – inflammatory medications.
- Other Painkillers – In patients that cannot tolerate NSAIDs due to side effects or other concurrent illness there are other classes of painkiller may be needed, for example paracetamol, tramadol, gabapentin and amantadine. Most of these have no animal licensed product for long term use but human preparations are widely used (off license) to provide effective pain relief. These drugs are also sometimes needed for additional pain relief in cases with severe clinical signs. Always seek advice from your veterinary surgeon before giving any human medications as doses may vary and some can be very toxic (for example ibuprofen).
- Complimentary Therapy – techniques such as acupuncture can have beneficial effects on mobility in some patients. Animals need to be referred to a trained veterinary acupuncture therapist for this.
- Physiotherapy – this can be used to improve mobility and maintain muscle tone
- Surgical Treatment – for some specific joints there are surgical options for treatment. Hip and elbow replacements are available for severely arthritic joints. Lameness from stifle cruciate injuries can be helped by surgery to stabilise the joint but eventually a degree of arthritis will develop. Some painful arthritic joints can benefit from debridement of the cartilage either by arthroscopy or surgical opening of the joint. In young dogs with lameness due to developmental defects in cartilage (OCD) arthroscopy can be used to remove painful bone fragments and cartilage flaps.
- Stem Cell Joint Injections – a new area being investigated for treatment is the injection of stem cells into arthritic joints. These are the precursor cells to producing the normal joint tissues including cartilage and can be harvested from the animals own fatty tissue. They are then multiplied in a laboratory and prepared for introduction to the joint. While good results have been achieved it is only of benefit to certain cases. Our visiting orthopaedic specialist, Ben Walton, is happy to discuss whether this treatment would be appropriate for specific patients
- Laser Therapy – there is anecdotal reports of this helping some patients but currently there is not much scientific evidence of benefits
- Monoclonal Antibody Therapy – this is a newly developed form of therapy where monoclonal antibodies are given by monthly injection under the skin. The antibodies target nerve growth factor in joints to reduce pain and inflammation. Trials have been very encouraging and suggest this may be a safe, effective alternative to more traditional treatments. The injection for dogs is called Librela.
Hydrotherapy
Sessions in the pool with experienced hydro therapists help hugely with rehabilitation and increase the chance of a successful return to full fitness. Hydrotherapy is also beneficial in young growing dogs with developmental conditions.
Supervised sessions in the pool helps to ease pain and increase mobility of dogs with arthritis as discussed in our Arthritis article.
It will also increase fitness in Sporting dogs and can be very beneficial in dogs needing to lose weight.
We have worked in partnership for over 14 years, referring dogs to the North Wales Canine Hydrotherapy Unit in Abergele.
Tony and Pauline have always been very helpful and professional and feedback from clients has been 100% positive.
Visit their website on www.swimyourdog.co.uk or see details on our Useful Contacts page.






